5 Overview of clinical placement experience
Clinical placements are a highly valued learning experience. Good preparation is essential to get the best from your clinical placement experience. Clinical placements are offered as real-world experiences in actual clinical settings alongside the nursing and midwifery workforce within teams dealing with real clinical problems. Your clinical placements will also include opportunities to experience nursing practice as a member of a multidisciplinary team, including learning alongside or being supervised by other medical and allied health professionals. Good preparation is essential to get the best from your clinical placement experience. This includes preparation for different work hours to what you and your family may be familiar with – including rotating shifts, weekends, and public holidays.
Students attend a clinical setting for a supervised clinical experience as part of a specific unit. Individual unit information, set out in each Learnline site, describes the purpose and assessments associated with each clinical placement.
| A clinical placement can only be provided via the Placement Office. |
| See your Learnline Unit for the requirements, purpose, and assessment documentation to be submitted for each clinical placement. |
| A clinical placement must be undertaken within 12 months of the clinical teaching block/simulation block. |
Bachelor of Nursing (course code BNRSG)
There are five units in the Bachelor of Nursing program that include specific clinical placements. Three of these require attendance at on-campus clinical teaching blocks. These are shown in the table below.
Table 2. Units with clinical placements in the Bachelor of Nursing (BNRSG)
| Clinical Placement Unit | Components |
| NUR125: Nursing Practice 1 | Theory
4-day clinical teaching block 160 hours clinical placement in sub-acute setting |
| NUR244: Nursing Practice 2 | Theory
4-day clinical teaching block 160 hours clinical placement in an acute setting |
| NUR343: Nursing Practice 3 | Theory
4-day clinical teaching block 160 hours clinical placement in an acute setting plus 80 hours in mental health setting |
| NUR344: Nursing Practice 4 | Theory
160 hours clinical community setting |
| NUR346: Transition to Practice 2 | Theory
160 hours clinical placement in a primary, secondary or tertiary setting |
Bachelor of Midwifery (course code WMIDW1)
There are eight units in the Bachelor of Midwifery that include specific clinical placements. Four of these include on-campus clinical teaching blocks. Additionally, Midwifery students must complete continuity of care experiences. These are shown in the table below.
Table 3. Units with clinical placements in the Bachelor of Midwifery (WMIDW1)
| Title of Clinical Placement Unit | Components |
| MID101 Introduction to Professional Midwifery Practice | 32 hours clinical teaching block
80 hours clinical placement |
| MID102 Fundamental Skills for Midwifery Practice | 32 hours clinical teaching block
120 hours clinical placement |
| MID202 Professional Midwifery Practice 1
Co-requisite unit MID201 |
32 hours clinical teaching block
240 hours clinical placement |
| MID204 Professional Midwifery Practice 2
Co-requisite unit MID203 |
240 hours clinical placement |
| MID301Women’s Health | 80 hours clinical placement |
| MID303 Professional Midwifery Practice 3
Co-requisite unit MID302 |
32 hours clinical teaching block
240 hours clinical placement |
| MID306 Professional Midwifery Practice 4
Co-requisite unit MID305 |
240 hours clinical placement |
| MID307 Specialist Neonatal Care | 120 hours clinical placement |
| Continuity of Care Requirement | Students are required to complete 10 CoCs by the end of the Bachelor of Midwifery course.
Students MUST attend their first placement before initiating any CoC relationships. |
The Placement Office
The Placement Office is responsible for all administrative aspects of arranging clinical placements. The Placement Office arranges and maintains agreements between health care providers and the College.
You are not permitted to arrange your own placements (or make up shifts). If a health facility offers you a placement (e.g. as an employer), thank them, obtain the contact details and email address, and provide these to your Placement Officer for follow up.
Booking your clinical placement
Time away from family, childcare, and employment leave arrangements can make the task of attending clinical placement complex. Travel of two hours away from home or even interstate may be required. Careful preparation is necessary before booking the placement as non-attendance will have a significant impact on your course progression.
When you are ready to nominate for your simulation block, log in to check your pre-clinical status with your login and password.
You will be notified by email approximately four weeks prior of the details of the clinical placement with details of when and how to contact the health facility prior to placement. Remember that official emails from the university are sent to your student email address.
Requests to change your clinical placement
Generally, a request to make changes to the offered clinical placement is not possible; this includes changes to dates, days, shift work, and geographical locations.
The College understands life circumstances can intervene unexpectedly, are outside of your control, and you may find you are unable to accept the offer made to you for clinical placement. This can include notification of military deployment, employer cancels leave, etc. (for issues related to illness see “reasons for absence” below)
Where circumstances have changed such that you are no longer able to undertake clinical placements as they are normally offered, a discussion with Access and Inclusion may assist.
If you need to decline the placement offered to you, you will need to contact your Unit Coordinator to discuss the issues. Your Unit Coordinator will notify the Placement Office and the offer of placement will be provided to another student.
You should be aware that declining a clinical placement means you return to the placement request queue as a new request. Therefore, you will need to re-enroll into a later semester that matches better with your availability. These changes delay your progression.
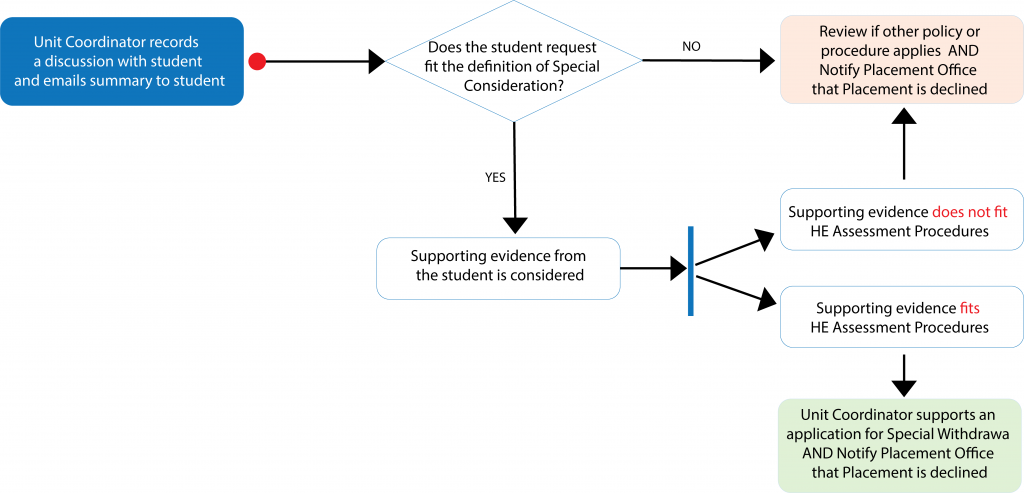
A decision to support a withdrawal without penalty will be based upon the Higher Education Assessment Procedures under Special Consideration. You will need to provide supporting evidence will be requested to support a decision.
Lateness, illness and other reasons for absence
The health facility expects you to attend the clinical placement booked on your behalf by the Placement Office at the allocated shift start time. Health facilities make operational decisions based on your attendance. Normal operational processes for absence apply to you. Additionally, your assessment requires clinical placement hours to be accounted for. The required clinical placement hours are set out in your Learnline Unit assessment details.
If you are unable to attend a booked placement, you may be able to make an application for a special withdrawal from the unit if exceptional circumstances apply (documented evidence will be needed). Otherwise, non-attendance means mandatory hours and assessments are unable to be successfully completed, resulting in a fail grade for the unit.
Lateness or absence – for example, traffic accident or illness – can be unexpected. You should identify on the first day of placement the number to call and the process expected of you by the Facility should you be late or absent. It is a professional responsibility to inform your supervisor if you are going to be late or will be unable to attend a rostered shift.
Illness, such as the “flu” or flu-like symptoms, is ordinarily problematic as a student. However, when attending clinical placement you must also consider the infection risk to your patients or clients. Until you are medically cleared you must not put your clients or patients at risk. Infection can have very serious consequences. If you are unwell or have symptoms that indicate you are unwell you should not attend clinical placement until your medical practitioner clears you or completely symptom free.
| See also Australian Government information on coronavirus (COVID-19) signs and symptoms and risks and actions being taken within the health sector. |
If you are uncertain what to do, contact your medical practitioner or the clinical supervisor in the health facility before attending.
If you are unable to attend placement due to illness or other reason, you must:
- Notify the Health Facility prior to the shift commencing;
- Contact the Placement Office and your Unit Coordinator as soon as possible;
- Obtain a Medical Certificate if unwell, or complete a Statutory Declaration to account for missed hours. A copy must be provided to the Placement Office and the Unit Coordinator. Attach an additional copy to your Clinical Assessment Portfolio.
- The Placement Office will liaise with you and the Health Facility to secure appropriate make-up time on your behalf.
Severe weather events
The personal safety of students is the primary factor in the event of a cyclone or other severe weather event. Closure of schools and other related factors may prevent attendance.
If there is an official decision to close Charles Darwin University Casuarina and Palmerston campuses due to a cyclone the student should contact the Health Facility and advise that they are unable to attend clinical placement until the University re-opens. Students in other locations should continue their placements as required and contact staff at the Alice Springs or Sydney campuses until the Casuarina campus reopens. Prior to closing the Placement Office will make every reasonable effort to advise students who they can contact if the need arises.
If absent due to weather events, the Placement Office will prioritise organisation of “make up” shifts and do their best to minimise any inconvenience to students.
Expected student behaviour on clinical placements
The health facility expects you to act professionally at all times, and comply with the policies of the organisation. In return, you are provided with a supervised opportunity to learn. The expected behaviours of a student working towards the registered nurse or registered midwife standards are set out in your Clinical Assessment Portfolio. Remember that you must comply with the policies and procedures of the health facility. Breach of confidentiality, including via social media, is regarded as a serious event by the health facility, the university, and the patient concerned.
You should also be aware of the following expectations health facilities generally have about students:
- Be respectful, courteous and professional at all times to colleagues, supervisors, clients/patients, Health Facility staff, and the public;
- Comply with the policies and procedures of the Health Facility; this includes respecting and promoting the Mission Statement of the facility;
- Obtain an orientation to emergency and evacuation procedures;
- Practice under the supervision of the clinical staff;
- Be fit for undertaking clinical practice, including maintaining own health and ensuring adequate rest;
- Notify your supervisor if you become unwell, and also if experiencing symptoms indicating you may be unwell (e.g. flu-like symptoms, etc.);
- That you understand and practice within your student Scope of Practice (see the Clinical Assessment Portfolio);
- Take responsibility for your own learning and are motivated to seeking out learning opportunities as well as assist in general clinical tasks and routines;
- Be punctual – arriving at least 15 minutes prior to commencement of an allocated shift and returning from meal breaks on time;
- Speak English at all times while on site or while ever in your role as a student nurse or midwife;
- Wear the Charles Darwin University uniform and your name badge above the waist in a location easily visible unless specifically directed otherwise by the Health Facility;
- Inform the Registered Nurse or Midwife responsible for client care in the area whenever leaving the area;
- Report any malfunction or breakage of equipment and any health and safety hazards to the Registered Nurse or Midwife responsible for client care in the area;
- Be sensitive to and respectful of client’s physical and cultural safety;
If at any time your clinical supervisor or the facility judge that they are unable to provide sufficient supervision, or for operational reasons can no longer provide supervision, the facility can request the clinical placement be terminated.
Assessment on clinical placements
The primary purpose of your clinical placement is to gain experience applying your clinical reasoning, knowledge and skill to people in need of nursing or midwifery care. Assessment assists you to understand your progress and guides you toward meeting the required standards.
While on clinical placement, your progression toward the relevant NMBA Standards for Practice is assessed. Your Clinical Assessment Portfolio records these assessments and guides you and your supervisor through the aims and objectives of the placement, who must sign, when and how to submit. You will need to print a copy of the Clinical Assessment Portfolio prior to beginning the placement and be familiar with the requirements.
If you do not understand the assessment requirements, you should contact your Unit Coordinator.
| See your Learnline Unit for the requirements, purpose, and assessment documentation to be submitted for each clinical placement (e.g. Clinical Assessment Portfolio). |
Unsatisfactory progress
See the section about “Challenges on clinical placement” on page 15.
Supervision on clinical placement
As a student beginning your journey towards professional nursing practice, your clinical placement experience is an opportunity to begin to apply knowledge and skill within a real clinical setting. This always occurs under the supervision of an experienced Registered Nurse. On some placements you will have the opportunity to also undertake experiences supervised by medical or allied health professionals.
Supervision may be arranged in different ways at different health care facilities, or may be different according to different specialty areas. The level of supervision also changes as you progress through your course and demonstrate competence to take on increasing responsibility. Initially, you may find the different terms used for your supervision to be confusing.
In most organisations, your clinical placement experience will be overseen by a Clinical Nurse Educator or Clinical Facilitator who is responsible for a group of students at the facility. Where this model is provided at the health facility, you will find that you are then allocated a Registered Nurse who will be your preceptor for each shift or across a sequence of shifts.
In some placements, you will have an opportunity to accompany a clinician from a different discipline (e.g. Aboriginal Health Worker). The allied health professional will sometimes be referred to as your clinical supervisor. Nonetheless, your Clinical Nurse Educator or Clinical Facilitator retains overall responsibility for your clinical placement and will ensure that a Registered Nurse assesses signs off on your practice. They will do so in consultation with the interdisciplinary clinical supervisor.
At smaller facilities, the Clinical Facilitator may also be the person who supervises you for some or all of your clinical placement. Alternatively, you may encounter arrangements where your Clinical Facilitation is shared among two or three key senior nursing staff. While this may seem a cumbersome arrangement, students often find that smaller health facilities can offer a range of personalised learning experiences not possible in very large health care settings.
A Clinical Facilitator may be an employee of the health service or directly contracted by the College of Nursing and Midwifery. The Clinical Facilitator is responsible for your orientation to the facility, key policies and procedures and any specific risks. They may do this themselves, or may delegate this to a preceptor.
The Facilitator is also responsible for guiding the quality of your overall learning experience. They will frequently check in with you each day to ensure your learning experience is progressing. These check-ins are useful times to reflect on your practice development, communication skills and application of knowledge to clinical problems. As you develop as a student, a key feature will be developing skills with structured clinical reasoning.
Media Attributions
- Check your pre-clinical status © Denis Doan adapted by Charles Darwin University is licensed under a All Rights Reserved license
- Flowchart-for-placement-01 © Denis Doan adapted by CDU is licensed under a All Rights Reserved license
- Student nurse © iStock/Voysla adapted by Charles Darwin University is licensed under a All Rights Reserved license